.
DAISI began 2023 with a strategic and ambitious plan of one subspecialty surgical trip to the Solomon Islands every month.
.
This was on the request of previous Director of Medical Services Dr John Hue, and given official approval by the Solomon Islands Ministry of Health and Medical Services (MHMS). It was an ambitious plan, after pretty much no trip and only video conferences throughout the COVID outbreak. Like all ambitious plans, ours was no exception and challenges struck the second half of this year.
Beginning strong, DAISI was able to successfully send to the Solomon Islands one surgical subspecialty trip every month including the surgical subspecialities of urology, colorectal, hepatobiliary, and diabetic foot disease. However the second half of this year the “wheels began to fall off” this ambitious plan. Competing geopolitics and a growing focus on the Pacific Games scheduled to be hosted at Honiara in November 2023 resulted, disappointingly, in the last three DAISI trips to National Referral Hospital (NRH) and Gizo being cancelled. This was in large part due to funding issues within the Solomon Islands Ministry of Health and Medical Services (MHMS).
This forced DAISI to subsequently take a pause and reconsider its next approach. With this pause came the unfortunate resignation of DAISI Secretary Dr Gary McKay, with the Solomon Islands Programme Officer Professor Peter Hewett taking on this new challenging and somewhat daunting role.
Professor Hewett has been instrumental in getting the Solomon Island’s program back on track this year, with a fact finding & diplomacy visit late last year to establish this year’s ambitious curriculum.

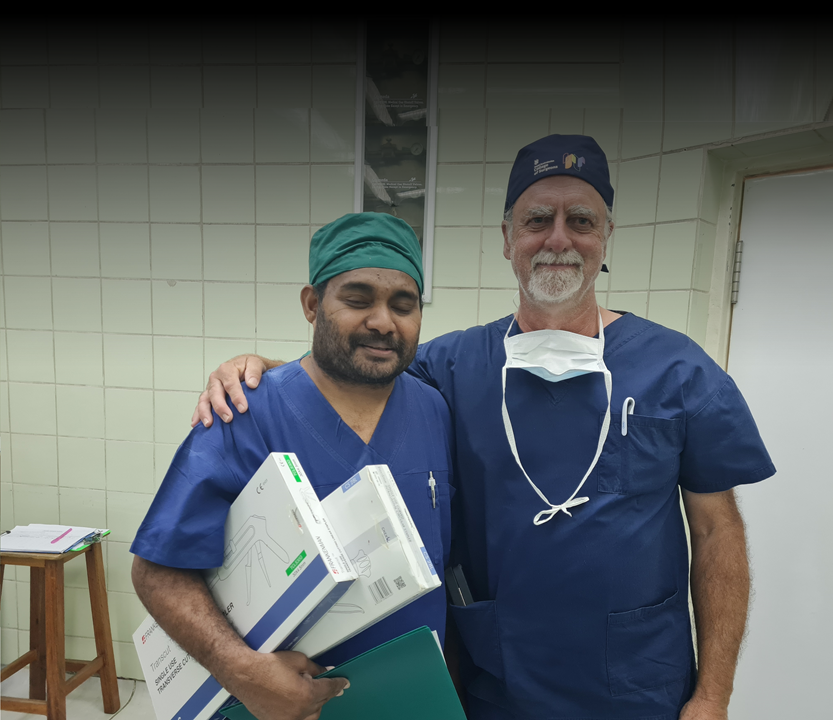
With all future DAISI trips cancelled, on request from the NRH surgeons in November this year, current DAISI Secretary Professor Peter Hewett travelled to Honiara to treat a glut of patients with rectal cancer. Initially eight patients which was reduced to five for the usual reasons (mostly advanced inoperable disease). All cases were advanced and required permanent or temporary stoma formation after resection. All patients recovered from their procedures and have been discharged from hospital. As part of the service provided, Dr Basil Scott Siota and Professor Peter Hewett performed the first laparoscopic stoma formation in the Solomon Islands.

Although technically not particularly difficult, the beauty of this operation is its simplicity, allowing a palliative bypass procedure and discharge home within a fairly short time frame due the avoidance of a large incision and major abdominal surgery. In the setting of many advanced inoperable cancers presenting to NRH, this is understandably a very useful operation for surgeons such as Dr Scott Siota, as well as new emerging surgeons, to add to their armamentarium. Professor Hewett was also able to replenish the supplies of stoma appliances courtesy of stomal therapist Amanda McGee RN from Adelaide, with a suitcase full of appliances carried in Professor Peter Hewett’s hand luggage.

The trip was in the shadow of the Pacific Games with the opening ceremony being held on the 19th November in the new 70-million-dollar stadium. The NRH has had some improvement work done on it in the last 12 months. A new Medical High Dependency Unit (HDU), funded by the Australian Government was opened earlier in 2023 by the Deputy Prime Minister the Honourable Richard Marles. It recently was used for postop supervision of neurosurgical patients who had been treated by an eighteen-strong Sydney neurosurgical team. A new surgical ward had been refurbished for possible use during the Pacific Games. This will be of benefit after the Games are complete.

Both America and China had hospital ships USSNS MERCY which arrived on the 16th of November to support the health system during the games and the Chinese naval hospital ship the PEACE ARK which visited on August 19th. Other areas had been improved and on recent verbal reports suggested that the New Zealand government had allocated funds for rat eradication at NRH.

Over 200 amputations continue to be performed in NRH the majority as a result of Diabetic Foot Disease. Education at a local level is a key factor in prevention. DAISI has been instrumental in coordinating efforts for training SI nurses and doctors (funded in the first instance by Irish Aid) and working with Professor Viv Chuter to introduce a nurse training module to Solomon Island University. Discussions with DFAT are ongoing with a comprehensive plan to be developed for a funding model in this area.

DAISI exists in a crowded aid environment in the Solomon islands with 22 different Aid teams attending in 2023. Francis Kennedy is now the aid team visit and medical student elective coordinator fkennedy@nrh.gov.sb All future DAISI visits will be flagged with Francis.
Education remains a major priority for further development. Areas include Oncology services, Breast Cancer Surgery and treatment update, and a general overview of treatment guidelines and advances in general surgery subspecialties suited to a recent successful Australian fellowship candidate who could spare a week to provide education at NRH. Professor Desmond Yip from Canberra Hospital has been integral to the establishment of an oncology service at NRH in partnership with local medical oncology trainee Dr Andrew Soma.

Combined with new CT scanner technology, oncology services are now entering an exiting new phase being able to both provide chemotherapy treatment and monitor for signs of response and recurrence.
In regard to education, a mention should be made of Dr Maddie Gramlick a 4th year SET trainee funded by AVI, who has spent the last 4 months organising the logistics of laparoscopic surgery in NRH. She has successfully launched a training program for the local surgical registrars in diagnostic laparoscopy and laparoscopic appendicectomy. Importantly three laparoscopic towers and equipment have been donated by the USSNS MERCY to the NRH giving an increased opportunity to advance laparoscopy in this setting. Dr Gramlick is leaving her position shortly but through DAISI will continue her work in the Solomon Islands.
Next year will be interesting. With the excitement of the Pacific Games over, it is hoped once the dust settles that DAISI will be able to re-establish a reliable and comprehensive program again in partnership with the Solomon Islands Ministry of Health and Medical Services (MHMS). The role of planned versus ad-hoc visits on invitation remains a subject for discussion with both having merit: planned trips give certainty to allow cases to be booked in advance, whereas ad hoc lists respond to the current demand. Next year there will probably be an ongoing role for both style of visits with a certain degree of flexibility needed to get the mix just right!
Author: Dr Sepehr Lajevardi is a plastic surgeon from Sydney and a founding member of DAISI, currently sitting on the DAISI Board.