
National Referral Hospital Surgical Outreach Team (NRHSOT) surgeon Dr Scott Siota doing key hole surgery through small incisions with DAISI volunteer surgeon Prof Charbel Sandroussi.
We’ve all heard it said that prevention is better than cure. When it comes to good health, there is no substitute for a healthy diet and lifestyle. Many diseases and cancers can be prevented by simple measures such as increasing dietary nutrition, avoiding obesity regular exercise and refraining from certain known carcinogens found in cigarettes, alcohol and beetle nut. Sometimes, despite this, disease or cancer still occurs. This is when early detection and treatment is vitally important. The fifty plus age group represent a population most at risk for cardiac and diabetic disease and many cancers. Cancers, if diagnosed early, can be removed far more easily and successfully that if diagnosed late and hence the phrase “a stitch in time saves nine”. Self-performed breast examination once a month can easily pick up a new small breast lump that can be removed surgically before it spreads. Bowel cancer may present in its early stages with streaks of blood within the stool, or even a change in bowel habit and sudden constipation. Colonoscopy is a quick, non invasive procedure that can diagnose bowel cancer early allowing surgical treatment alone to cure this disease. This is available at both National Referral Hospital (NRH) and Gizo hospital. Thyroid cancer and head and neck cancer, particularly oral and lip cancer, is common in the Solomon Islands, and is first noticed by a small ulcer or lump that doesn’t heal or disappear over time.
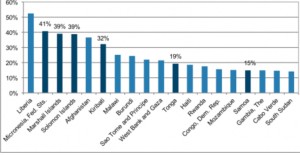
Over the past 100 years, medical aid in the Solomon Islands has largely been reactionary, treating disease once it occurs. It is only in the last 20 years that significant strategies in preventative medicine have been made. Infectious diseases such as malaria, dengue fever and tuberculosis are less common than twenty years ago, but still remain a challenge, with significant medical funding currently tackling these in a preventative manner. Medical service delivery has also, for most of the past century, been mismatched with a focus on tertiary hospital care rather than preventative medicine or early detection of disease. More than 80% of doctors are in the capital Honiara and only 20% of doctors are in rural provincial hospitals, where the need is the greatest, with these hospitals covering over 85% of the population.
The ministry of health’s ambitious policy of universal health coverage known as the Role Delineation Policy (RDP) will bring better health coverage to the majority of the population who are deprived of care that is available only in urban centres. The RDP defines what level of facility, human resources and services will be provided at different levels of care, from community health centres to rural health centres, to area health centres to provincial hospitals. The policy proposes that larger area health centres will have a resident medical doctor and dentist with imaging, laboratory and procedural facilities. The idea once fully implemented in a few years will revolutionise health care service provision to the rural population, and will see a reduction in the late presentation of disease being referred to Honiara.
Currently, specialist surgeons and gynaecologists from Honiara’s National Referral Hospital Surgical Outreach Team (NRHSOT) are visiting provincial health centres to provide screening and surgery to these remote centres. This not only provides service delivery where it is most required, but represents major cost savings in avoiding unnecessary transfer of patients to Honiara for their surgery or treatment. Over the past year, over 400 operations have been performed by NRHSOT visits to remote provincial hospitals including Gizo, Kilu ‘ufi, Kirakira and Munda. These teams are led by senior specialist surgeons from Honiara, and often supported by volunteer specialists from abroad, providing highly sophisticated specialist surgery. In the last year, Gizo hospital and National Referral Hospital (NRH) have been offering key hole (laparoscopic) surgery, and endoscopy (gastroscopy and colonoscopy) for early disease and cancer. These minimally invasive procedures can avoid the need for a large operation or incision. However getting the message to the community is often the hardest challenge to the success of these fly-in fly-out missions, with screening of suitable patients for surgery usually conducted the first day of a one week visit. With greater awareness by the community of when these visits are scheduled to happen, it is hoped that all in the community can benefit from these NRHSOT visits.
Screening for surgical cases (thyroid, breast lumps, hernia, colorectal conditions, early symptoms of bowel cancer such as blood mixed in stool) will occur at Gizo hospital from 10am – 2pm on Monday 25th September, and Tuesday 27th February. Screening will occur at from 10am-2pm on Thursday 8th November at Kirakira hospital. Surgery and screening colonoscopy and gastroscopy will then be conducted that same visit with visits usually one week in duration.
Dr Sepehr Lajevardi is Treasuer of DAISI, and is a plastic surgery registrar who has participated in a number of visits to Gizo hospital over the past three years.














 In addition to over 8 pallets of surgical scrubs, the container also included linen, overalls, warming jackets, and theatre dresses. It is hoped that this large volume of scrubs and linen will be circulated to each of the hospitals in the Solomon Islands.
In addition to over 8 pallets of surgical scrubs, the container also included linen, overalls, warming jackets, and theatre dresses. It is hoped that this large volume of scrubs and linen will be circulated to each of the hospitals in the Solomon Islands.
